Researchers in the United States and China have recently released data from a study of the oral microbiome suggesting that the type and abundance of bacteria found in the mouth may be linked to lung cancer risk in nonsmokers. The study, which Albert Einstein College of Medicine assistant professor, H. Dean Hosgood, Ph.D., and colleagues said is the first of its kind, indicated that fewer species and higher numbers of particular types of oral bacteria seemed to be linked to heightened risk of lung cancer.
Reporting their results in Thorax (“Variation in oral microbiome is associated with future risk of lung cancer among never-smokers”), the researchers acknowledged that further work will be needed to further understand the role of oral and respiratory tract microbiota in respiratory diseases. Nevertheless, they concluded, “Our observed associations highlight the importance of the microbial richness, and the potential relevance of rarer taxa, in relation to the risk of lung cancer.”
Lung cancer is the leading cause of cancer-related death. While the link between tobacco smoking and lung cancer is well known, one in four cases of the disease occur in nonsmokers, and such cases represent the seventh leading cause of cancer death globally, they continued. “Known lung cancer risk factors such as active tobacco smoke, second hand tobacco smoke, radon, household air pollution, outdoor air pollution, and family history of lung cancer do not fully account for the disease burden.”
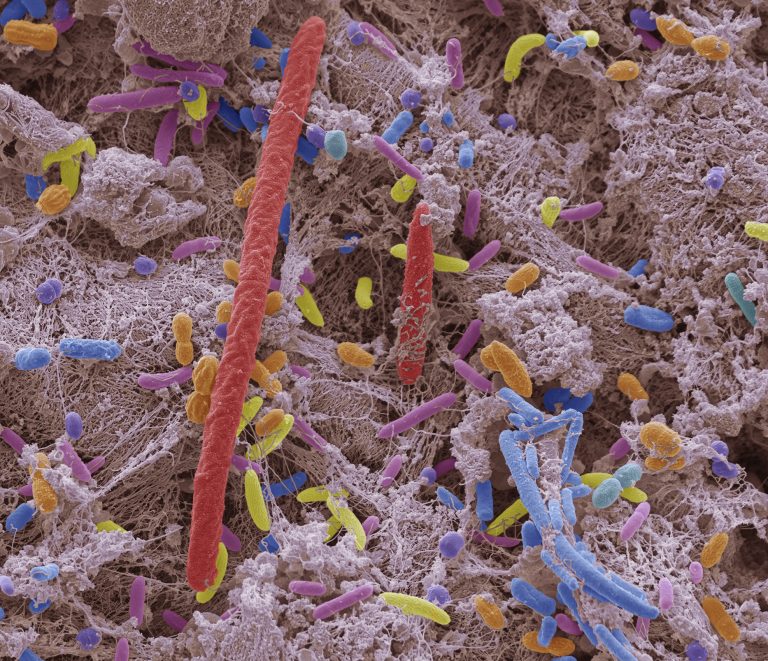
The human microbiome refers collectively to the communities of commensal microorganisms, including bacteria, fungi, and viruses that live on and in our bodies, particularly on the skin, and in our oral cavity and gastrointestinal tract. Not only do such microorganisms outnumber human cells, but they collectively encode 100-fold more genes than the human genome, the authors noted. “The diversity and abundance of bacterial communities within the body have led to the microbiota being referred to as the ’11th organ,’ with potential influences on human health and diseases.”
Previous research has found associations between gastrointestinal tract cancers and the gut microbiome, and has also linked the type and volume of bacteria found in the mouth with a heightened risk of various cancers, including pancreatic cancer. One recent prospective study found an association between increased abundance of oral commensal bacteria, and a lower risk for a type of head and neck cancer, “… providing evidence that microbiota outside the gut may also be associated with cancer risk,” the team noted.
The investigators wanted to find out if there might also be a link between the oral microbiome and lung cancer, given that the mouth represents an entry point for bacteria to the lungs. Bacterial communities have previously been detected in lung tissues, and may be linked with the risk of non-malignant and malignant respiratory disorders, they suggested. “For example, differences in lung bacterial flora have been found between patients with severe chronic obstructive pulmonary disease (COPD) and those with non-diseased lungs.”
For their study reported in Thorax, the researchers turned to participants in the Shanghai Women’s Health Study and the Shanghai Men’s Health Study, all of whom were lifelong nonsmokers, and whose health was monitored every 2 to 3 years after entry to the study, between 1996 and 2006. “This is the first report of a prospective study of the oral microbiome and lung cancer risk among never-smokers,” the team wrote.
At enrollment, participants rinsed out their mouths to provide a profile of the resident bacteria, and information was obtained on lifestyle, diet, medical history and other environmental and workplace factors that might influence their disease risk. The team carried out metagenomic shotgun sequencing to evaluate bacterial diversity and abundance, at this baseline point.
Overall, 90 of the women and 24 of the men in the trial went on to develop lung cancer within seven years, on average. These cases were then matched with 114 nonsmokers of the same age and sex, who didn’t develop lung cancer, but who had similar levels of education and family histories of lung cancer. These control participants also provided a mouth rinse sample.
Comparison of both sets of rinse samples showed differences between the microbiomes of participants in the two groups. The results suggested that a wider range of bacterial species was associated with a lower risk of developing lung cancer, and a larger volume of particular types of species was also associated with lung cancer risk. A greater volume of Bacteroidetes and Spirochaetes species was associated with lower risk while a larger volume of Firmicutes species was associated with heightened risk of lung cancer.
Specifically, within the Spirochaetes species, a greater abundance of Spirochaetia was associated with lower risk; and within the Firmicutes species, a larger volume of organisms from the Lactobacillales order of microbes was associated with a heightened risk.
The associations remained when the analysis was restricted to those participants who had not recently taken any antibiotics prior to sample collection, and after excluding individuals diagnosed with lung cancer a relatively short time after they gave their samples. “The robustness of our findings is exemplified by the associations remaining after excluding individuals who used antibiotics during the seven days prior to sample collection, as well as after excluding individuals who were diagnosed with lung cancer shortly (e.g., within two years) after the baseline sample was collected,” the scientists wrote.
They acknowledged that their observational study wasn’t powered to establish cause, and noted several limitations. “While our study provides evidence that variation in the oral microbiome plays a role in lung cancer risk, the interpretation of our study must be done while considering the caveat that our findings are from a single time point in a single geographical location,” they noted.
Nevertheless, the scientists pointed out, in a previous, retrospective case-control study of never-smoking women in China, they also found a link between lower bacterial α-diversity in sputum samples and increased risk of lung cancer. And notably, they continued, “Our findings regarding the abundance within the Bacteroidetes and Firmicutes phyla are in agreement with prior literature assessing the relationship between the microbiome and lung disease … When taken together, the limited but growing body of literature suggests that decreased microbial diversity and increased abundance of taxa within the Firmicutes phylum, and more specifically Lactobacillales, in the respiratory tract may be associated with an increased risk of lung cancer.”
In a linked editorial, Harvard University’s David Christiani, Ph.D., the Elkan Blout professor of environmental genetics, suggested that mouth bacteria may provoke chronic inflammation, boost cell proliferation and inhibit cell death, prompt DNA changes, and switch on cancer genes and their blood supply, which would help to explain the findings. While also noting the limitations of the study, Christiani commented, “… in light of careful adjustments for covariates collected in these populations, and the fact that these findings replicate those of smaller studies done earlier in another part of China in nonsmokers suggest that the results are robust and the observed loss of α-diversity, combined with specific taxa abundance may well play a mechanistic role in the genesis of lung cancer in nonsmokers.”
The study findings also raise several questions, he noted. “First, how stable is the human oral microbiome over time? Second, if the human oral microbiome varies over time, what determines that variability? Third, how does the ambient environment such as exposure to air pollutants, affect the oral (and lung) microbiome?”
It’s also not clear whether the oral microbiome as measured in this, and other epidemiological studies, represents a causative agent or only a marker of disease or immune activity, Christiani noted. “If it is the former, then it will be important to understand whether the oral microbiome actually seeds the lung microbiome and thus acts locally.”













