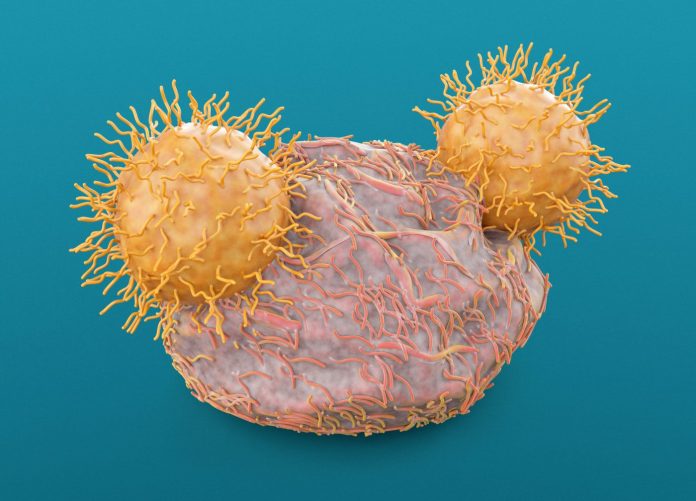
Researchers at the Massachusetts Institute of Technology (MIT) say they have used a vaccine that boosts CAR T therapy and it may be a method that can help this form of immunotherapy effectively treat solid tumors.
The MIT researchers have found a way to overcome one of the obstacles to CAR T therapy—its targeting of only one antigen—via a vaccine that both boosts the response of the engineered T cells, while also helping the immune system generate new T cells that target other tumor antigens.
The team’s work, published this week in the journal Cell, showed in mouse models that this approach made it more likely tumors could be eradicated.
“This vaccine boosting appears to drive a process called antigen spreading, wherein your own immune system collaborates with engineered CAR T cells to reject tumors in which not all of the cells express the antigen targeted by the CAR T cells,” said senior author Darrell Irvine, the Underwood-Prescott Professor with appointments in MIT’s departments of Biological Engineering and of Materials Science and Engineering.
The researchers believe this approach could help in the development of T cell treatments for cancers such as glioblastoma. Prior research for potential CAR T therapies for glioblastoma have targeted the mutated version of the EGFR receptor. But not all glioblastoma cells express this antigen, and some glioblastoma cells respond to the immune attack by stopping production of the CAR T-targeted antigen.
The new findings that showed the vaccine driving antigen spreading may help overcome this problem.
“That would be exactly the kind of thing that could help you deal with the antigen heterogeneity of solid tumors, because if you primed host T-cells to attack other antigens, they may be able to come in and kill the tumor cells that your CAR-T cells cannot,” Irvine noted.
For their study, the MIT investigators sought to discover how T-cell response is activated. Using the same type of EGFR targeting CAR T cell the team had used four years ago to study how applying a vaccine affected CAR T therapy against glioblastoma, they found that metabolic changes occurred in the CAR T cells that increased production of interferon gamma, a cytokine that helps stimulate an immune response. This activity helped T cells to overcome the immunosuppressive tumor environment that can shut down T cell activity.
The researches found that as CAR T cells killed tumor cells expressing the target antigen, host T cells encountered other antigens from those tumor cells which stimulated the host T cells to target those antigens to provide additional benefits in eradicating tumor cells. Lacking this response, the team noted that the tumors would regrow, even if the CAR T cells eliminated most of the original tumor cells.
Testing this combination in mice, the MIT investigators found that in tumors with only 50% of the tumor cells expressing the target antigen, that about 25% of the tumors could be eradicated by the combination of CAR T cells and the host T cells. And when there were greater levels of the target antigen, the success rate of this combination was even better. In cancer where 80% of the cells expressed the target antigen, tumors were eliminated in nearly 80% of the mice.
While the current study focused on treating glioblastoma and melanoma, the researchers noted it could potentially be used as a therapeutic approach for other tumor types. In addition, the team is now working to see if there are way to adapt CAR-T therapy so that is can be applied in instances where no targetable antigens have been identified.













