A Phase II clinical trial being led by researchers at Dana-Farber Cancer Institute along with 10 brain tumor centers across the U.S. is taking an efficient and innovative method to find new potential treatments for glioblastoma. While the adaptive platform trial has not shown any of the three therapeutics tested so far improved overall survival of patients, multi-arm trial, the first of its kind in neuro-oncology has the potential to quickly identify beneficial therapies for glioblastoma.
Results of the first data from the trial are reported in the Journal of Clinical Oncology and the trial called INSIGhT (Individualized Screening Trial of Innovative Glioblastoma Therapy), is ongoing and testing additional therapies
“There have been many failed attempts to find better therapies for glioblastoma,” says co-first author Rifaquat Rahman, MD, a radiation oncologist at Dana-Farber. “This new trial design meets a need for a more efficient and smarter way to find new therapies.”
Patients with glioblastoma have few effective treatment options. Those with a form of the disease called MGMT unmethylated glioblastoma fare the worst and rarely respond to the standard therapy of radiation plus chemotherapy.
Traditionally, investigational therapies for glioblastoma are tested either head-to-head against standard therapy, or on their own in a single-arm trial with no control arm. In contrast, INSIGhT uses a shared control arm to test multiple investigational therapies at the same time. To date, the trial has tested a control arm of standard therapy against abemaciclib (a CDK4/6 inhibitor), neratinib (an EGFR/HER2 inhibitor), and CC-115 (a DNA-PK/mTOR inhibitor).
“This design is more economical and faster than the alternative of three separate randomized phase 2 trials, which would require many more patients and a lot more resources,” says co-senior author and principal investigator Patrick Wen, MD, Director of the Center for Neuro-Oncology at Dana-Farber.
In this first analysis of results, the trial enrolled 237 patients with newly diagnosed MGMT unmethylated glioblastoma between 2017 and 2021. Initially, patients were randomly assigned to receive one of the four treatments. Each patient had an 25% chance of receiving any one of the four options.
Once underway, the trial adapts to new information. Dana-Farber statisticians led by Lorenzo Trippa, PhD, continuously apply complex statistics to learn from each patient whether the drug they are receiving is having a likely benefit. The randomization algorithms enables future patients joining the trial to have increased odds of getting the best drug for them personally.
For instance, if patients experienced toxicities or no signs of benefit from a treatment option, future patients would be less likely to receive that treatment. If another treatment option showed benefit to patients, future patients would be more likely to be assigned to that option. The algorithm also factors in biomarkers associated with a likely benefit from a given therapeutic.
This approach, called Bayesian Adaptive Randomization, reduces the number of patients exposed to therapies that are unlikely to be successful. It also helps researchers put resources into therapies with the most promise.
“We can quickly stop pursuing drugs that are not promising and at the same time find the effective drugs and move them into phase three testing,” says Wen.
At the same time, the trial has set up an infrastructure that helps researchers learn more about why patients respond or do not respond to the therapies. This is one of the first trials in neuro-oncology to require tumor genomic sequencing up-front for all patients, which helps researchers learn more about how genetic biomarkers influence responses.
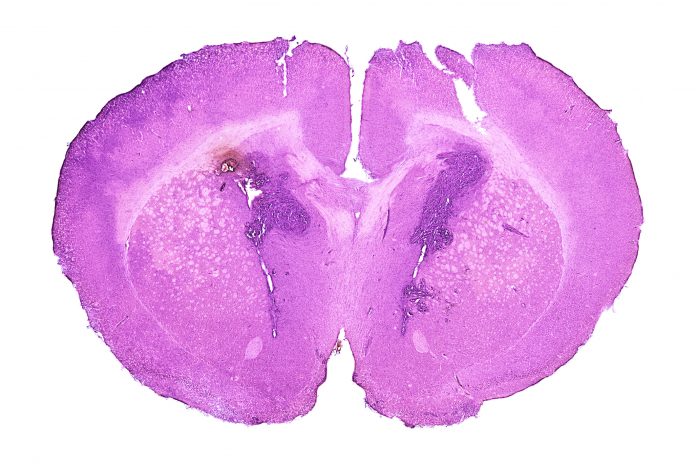
“It’s a very modern, science-enabling trial,” says co-senior author Keith Ligon, MD, PhD, a Dana-Farber pathologist and Chief of the Division of Neuropathology at Brigham and Women’s Hospital.
In this first readout of the trial, patients taking abemaciclib and neratinib experienced longer progression free survival than those receiving standard therapy or CC-115. None of the therapies extended overall survival.
The trial is designed to add new treatment arms and iss now currently assigning new patients to either a novel brain penetrant chemotherapy (QBS10070S), an immunotherapy regimen consisting of a tumor vaccine VBI-1901 and a PD1 antibody, or standard therapy.
Testing a drug that potential treatment for glioblastoma may be easier to do in the context of this trial because the trial is already established. Each new arm of the trial is an amendment to the trial, not a new trial itself.
“This trial is more streamlined, but it’s also rigorous, which makes it more likely that it will produce more reliable answers about whether or not a drug is worth further investment,” says Rahman.













