Needle biopsy is indispensable to the diagnosis, typing, and targeted treatment of breast cancer. A new study, however, indicates that the testing itself triggers a series of cell-level changes that promote the spread of the disease months later. The results are the first of their kind to suggest a mechanism for the observed increases in mortality in women whose surgeries are delayed more than the currently recommended 60 days. The study was conducted by researchers at the University of Oklahoma’s Stephenson Cancer Center and published in the 19 December 2023 issue of Cell Reports Medicine.
“Once a breast tumor is biopsied and wounded, a series of pro-metastatic changes occur in a relatively short period,” explained Takemi Tanaka, Ph.D., senior author of the paper. Tanaka and her colleagues used a multi-disciplinary approach, analyzing data on breast cancer patients and looking at the cellular changes that occur in both human and mice tumors following needle biopsy. In addition to evidence of a cellular mechanism, they found an even shorter biopsy-to-surgery safety window of 53 days. “Our study emphasizes the importance of timely surgery.”
The current study included a cohort analysis of patients with early estrogen receptor positive (ER+) breast cancer, as well as animal model studies looking at the mechanism of cancer cell dissemination following biopsy. “Our previous cohort study has shown that breast cancer progresses after 60 days of diagnostic biopsy in ER+ breast cancer,” she said. This observation raised the question of how slow-growing ER+ breast cancer progresses so quickly. Tanaka and her colleagues suspected needle biopsy may be accelerating disease progression and set out to test their hypothesis.
Tanaka’s team began by gathering data from the National Cancer Database on 176,481 patients with stage I-II stage breast cancer diagnosed by needle biopsy who had surgery as their first treatment between 2007 and 2017. They found an initial lag-phase of 43 days without a detectable increase in mortality risk compared to the reference group who waited 30 days for surgery. That changed to a significant increase in risk at 53 days.
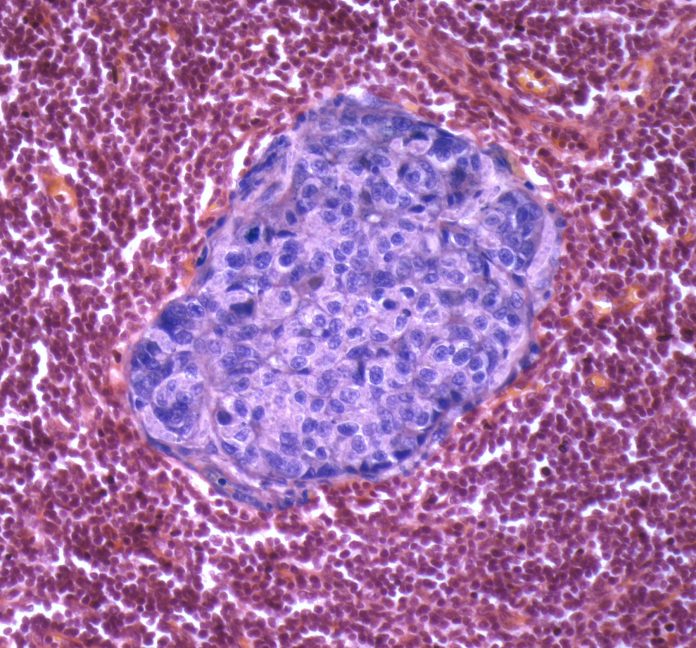
The researchers went on to study the wound sites of tumors from both humans and mice who underwent needle biopsy. They found what they describe as “biopsy-induced pro-metastatic changes” and for longer periods of time than normal wound healing. The changes included immune cells (macrophages), stem cell-like breast cancer cells, and angiogenesis, the growth of new blood vessels originating from the tumor.
The team also used the mice model to investigate the underlying mechanism that leads to cancer cell dispersion following biopsy. “Local invasion is a prerequisite for the systemic dissemination of cancer cells,” the researchers wrote in the paper. They performed needle biopsies on mice models of breast cancer. After 15 days, they found tumor-like cells in their lungs.
Taken together, the investigators concluded their results support the hypothesis that needle biopsy of ER+ breast cancer “provokes progressive pro-metastatic changes, which may explain the mortality risk posed by surgery delay after diagnosis.”
According to Tanaka, delaying surgery can have its benefits for the patient, allowing for genetic testing, MRI, fertility preservation, and second opinions. So, the team looked at the use of non-steroidal anti-inflammatory drugs (NSAIDs) as a possible treatment for biopsy wounding. They showed that oral administration of NSAIDs prevents biopsy-related disease progression in mice. “Our next step is to examine whether NSAIDs can be repurposed for the prevention of biopsy-related disease progression in humans,” Tanaka said. “We hope to implement safe and affordable pharmacologic prevention.”













