A new clinical tool, based on genetic mutations, blood cell parameters, and age, can identify patients with clonal hematopoiesis (CH) who are at greatest risk for developing a myeloid malignancy.
Details of the clonal hematopoiesis risk score (CHRS), developed by a team of researchers led by the Dana-Farber Cancer Institute, were presented at the 64th American Society of Hematology Annual Meeting in New Orleans.
Dana-Farber hematologist-oncologist and study lead author Lachelle D. Weeks, MD, PhD, told Inside Precision Medicine that clonal hematopoiesis is typically “identified incidentally in patients undergoing next-generation sequencing in the workup of low blood counts or when sequencing is performed to evaluate for solid malignancies or hereditary cancer syndromes.” It can also be detected in people participating in hematologic malignancy precursor registry studies, but screening is not currently recommended outside of these settings.
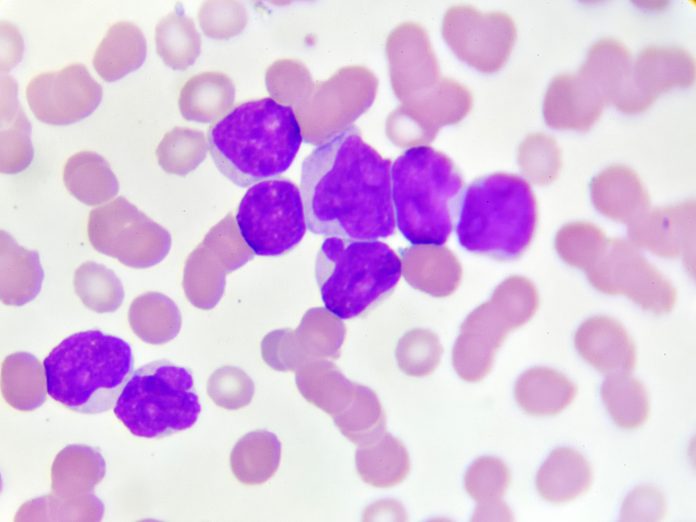
CH is a precursor of myeloid malignancies such as myelodysplastic syndrome (MDS), acute myeloid leukemia (AML), and the myeloproliferative neoplasms. It is present in around 15% of people over age 65 years, but only a small proportion, approximately 4%, will develop malignancies.
However, the lack of a robust, rigorous way to assess risk has meant that clinicians have struggled to advise CH patients on what the future could hold.
“As a provider who cares for these patients, I know first-hand that this is something that patients want to know. Patients want to know more than that they are at risk for a blood cancer, they want to know is that risk high and something I need to worry about or is it actually really low and not something that needs to be on the forefront of my mind,” said Weeks.
She added: “The CHRS is the first tool that we have that allows us to give patients an estimate of their risk in this way.”
To develop the tool, Weeks and her colleagues examined exome sequencing data from 193,743 healthy volunteer participants in the UK Biobank to determine specific genetic mutations associated with CH and then combined genetic data with other demographic and laboratory parameters. From this information, they identified several measures that were highly predictive of blood cancer risk in CH patients including patient age, genetic mutations associated with CH (single DNMT3A mutation, high risk mutations, multiple mutations), high variant allele frequency, and high red blood cell indices (red cell distribution width and mean corpuscular volume).
The researchers then combined these measures in a computational algorithm, creating a tool that calculates the CHRS and predicts an individual’s future risk for a myeloid malignancy.
The CHRS categorizes patients into three groups according to the likelihood of cancer progression—low risk (a score less than or equal to 9.5); intermediate risk (a score ranging from 10 to 12); and high risk (a score of 12.5 or greater).
In the UK Biobank cohort, 11,337 (5.9%) participants met the criteria for the two subtypes of clonal hematopoeisis, namely clonal hematopoiesis of indeterminate potential (CHIP) where no cytopenia is present and clonal cytopenia of uncertain significance (CCUS). The majority (87.6%) of these were categorized as low risk by the CHRS, with 11.3% intermediate risk and just 1.1% high risk.
In the patients with CHIP, the 10-year risks for blood cancer were 0.2% in the low-risk group, 2.6% in the intermediate-risk group, and 23.6% in the high-risk group. For those with CCUS, the risks were higher at 0.67%, 7.3%, and 50.6%, respectively. For the 182,406 individuals without CHIP or CCUS, the 10-year cumulative incidence of myeloid neoplasia was 0.2%.
The team validated their tool using three additional cohorts: a second cohort of roughly 250,000 healthy UK Biobank participants as well as two CH patient cohorts evaluated for hematologic conditions at the Dana-Farber Cancer Institute and the University of Pavia in Italy.
In the Dana-Farber Cancer Institute cohort, which included patients with both CHIP and CCUS, the overall incidence of myeloid neoplasms was 4.8%, while in the Pavia cohort, which consisted of people with CCUS only, the rate was 34.3%, underscoring the enhanced risk for progression in CCUS relative to CHIP. In both groups, the majority of patients who progressed to cancer were classified as high risk by the CHRS.
“In addition to helping us provide more information to patients, the CHRS will also serve as a unifying benchmark for defining which individuals with CH are highest risk for progression to overt malignancy like MDS or AML,” said Woods. “This is important because these are the patients who will derive the most benefit from clinical trials of therapies that are trying to prevent MDS and AML from developing.”













