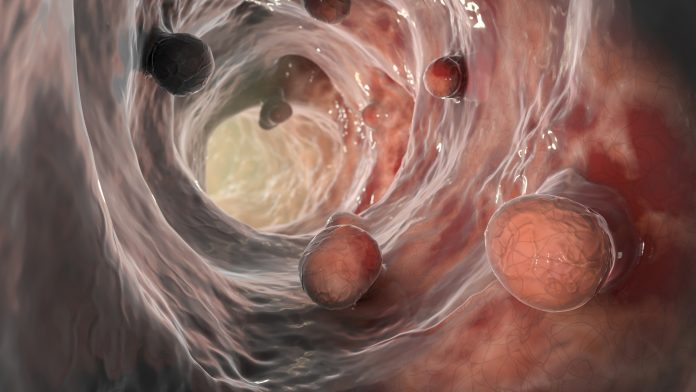
Prior studies have linked high blood cholesterol levels to various cancers, including colorectal cancers. However, it hasn’t been clear that lowering cholesterol can prevent colorectal cancers. Now, researchers at Weill Cornell Medicine have found in mice hard-to-detect colorectal pre-cancerous lesions known as serrated polyps, and the aggressive tumors that develop from them, depend heavily on the ramped-up production of cholesterol. Their finding points to the possibility of using cholesterol-lowering drugs to prevent or treat such tumors.
The findings are published in Nature Communications in an article titled, “Enhanced SREBP2-driven cholesterol biosynthesis by PKCλ/ι deficiency in intestinal epithelial cells promotes aggressive serrated tumorigenesis.”
“The metabolic and signaling pathways regulating aggressive mesenchymal colorectal cancer (CRC) initiation and progression through the serrated route are largely unknown,” the researchers wrote. “Although relatively well characterized as BRAF mutant cancers, their poor response to current targeted therapy, difficult preneoplastic detection, and challenging endoscopic resection make the identification of their metabolic requirements a priority. Here, we demonstrate that the phosphorylation of SCAP by the atypical PKC (aPKC), PKCλ/ι promotes its degradation and inhibits the processing and activation of SREBP2, the master regulator of cholesterol biosynthesis.”
The researchers analyzed mice that develop serrated polyps and tumors, detailing the chain of molecular events in these tissues that leads to increased cholesterol production.
“Serrated-type polyps and tumors currently are not treated differently from other colorectal neoplasias, but as our work shows, they have this specific metabolic vulnerability that can be targeted,” said study co-senior author Jorge Moscat, PhD, a Homer T. Hirst III professor of oncology in pathology, vice chair for cell and cancer pathobiology in the department of pathology and laboratory medicine and a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine.
The other co-senior author is Maria Diaz-Meco, PhD, a Homer T. Hirst III professor of oncology in pathology and a member of the Meyer Cancer Center at Weill Cornell Medicine. The study’s first author is Yu Muta, PhD, a postdoctoral associate in the Moscat/Diaz-Meco laboratories.
“Trials of statins to prevent colorectal cancer have had conflicting results,” said Diaz-Meco. “Our findings suggest that this is because targeting cholesterol has a preventive but selective effect only against polyps and tumors of this serrated type.”
The tumors that develop into serrated polyps account for roughly 15 to 30 percent of colorectal cancers, and contain many “metaplastic” cells that are particularly invasive and resistant to treatments.
Several years ago, the Moscat/Diaz-Meco team linked serrated polyps and tumors to low levels of two enzymes known as aPKCs. They showed that mice engineered to lack these aPKC enzymes in their gut linings reliably form serrated polyps and then aggressive tumors.
In the current study, the scientists found that in serrated-type tumors in these mice, and even in intestinal tissue, cholesterol synthesis was strikingly upregulated, suggesting that cholesterol may be an early driver of tumor development.
The researchers revealed how the absence of aPKC enzymes, especially in metaplastic tumor cells, unleashes the activation of a transcription factor called SREBP2, which switches on cholesterol production.
The results indicate that targeting cholesterol could be a viable strategy for treating and preventing serrated-type colorectal tumors. The Moscat and Diaz-Meco labs are now hoping to set up an initial clinical trial of a cholesterol-lowering intervention in patients from whom serrated colorectal polyps have been removed.
“Currently when these polyps are detected early with colonoscopy, they are removed and patients have to hope that they don’t come back,” Moscat said. “In the future, we hope to have a more active method to prevent this very aggressive form of cancer before it is fully developed and more difficult to treat.”











