Cerebrospinal fluid (CSF), the clear colorless liquid that protects the brain, also may be a factor that makes brain cancers resistant to treatment, according to new work from researchers led by Cedric Bardy at the South Australia Health and Medical Research Institute (SAHMRI) and Flinders University. Their study appeared last month in Science Advances.
The laboratory study also shows that trifluoperazine, a decades-old anti-anxiety drug, can improve the effectiveness of chemo-radiotherapy towards glioblastoma (GBM) cells, the most common and lethal brain cancer.
“We are raising funding to coordinate some clinical trials with patients with GBM,” Bardy told Inside Precision Medicine.
Brain cancers kill more children and adults under 40 than any other cancer. Brain tumors account for 85% to 90% of all primary central nervous system tumors. Worldwide, an estimated 308,102 people were diagnosed with a primary brain or spinal cord tumor in 2020. It is estimated that 5,230 children under the age of 20 will also be diagnosed with a CNS tumor in the United States alone in 2023.
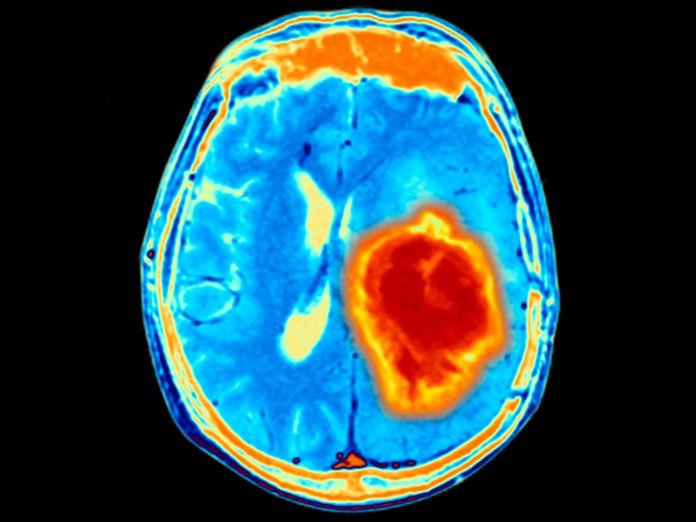
The most common primary malignancy of the central nervous system—GBM—has no cure. The current standard of care for this cancer is maximal surgical resection, followed by fractionated radiotherapy with concurrent and subsequent oral temozolomide chemotherapy. Despite this aggressive treatment, GBM tumors almost invariably recur and prove fatal. Median survival is about 15 months.
Since such tumors are resistant to therapies that kill cancers elsewhere in the body, this group of researchers speculates that unique features of the brain might contribute to the cancer’s resistance. The team comprised neurobiologists, neurosurgeons, and oncologists.
Previous studies that have looked at effect of blood, lymphatic vasculature, angiogenesis factors, cytokines, immune cells, and extracellular matrix on cancer cells in GBM have demonstrated the important role the microenvironment plays in cancer progression, plasticity, and treatment resistance. However, the primary base of the CNS microenvironment is cerebrospinal fluid (CSF), and its effect on cancer progression and treatment resistance is poorly understood.
This team tested the effect of human cerebrospinal fluid on the growth of tumor cells collected from 25 local patients with glioblastoma. Among the researchers’ findings, after exposure to CFS, the tumor cells quickly changed and became more resistant to both radiation and temozolomide.
Bardy says, “Glioblastoma kills so many people who are otherwise fit, healthy and young, within months. This is a horrible disease, and the treatments available are just not effective enough despite serious side effects.
“This study helps us understand the limitations of the current chemotherapies and provides new hope for repurposing a class of drugs that could be added to the standard of care.”
Investigating the molecular basis for these changes, the team found glioblastoma cells exposed to cerebrospinal fluid were more resistant to ferroptosis, a form of therapy-induced cell death. They identified nuclear protein 1 (NUPR1), a transcription factor hampering ferroptosis, as a mediator of therapeutic resistance in CSF.
Importantly, they also showed that trifluoperazine, an anti-anxiety drug used since the 1950s, could re-sensitise glioblastoma cells to both therapies. In contrast, trifluoperazine was found not to harm healthy brain cells. The researchers concluded that combining trifluoperazine with standard care may improve GBM patient survival.













