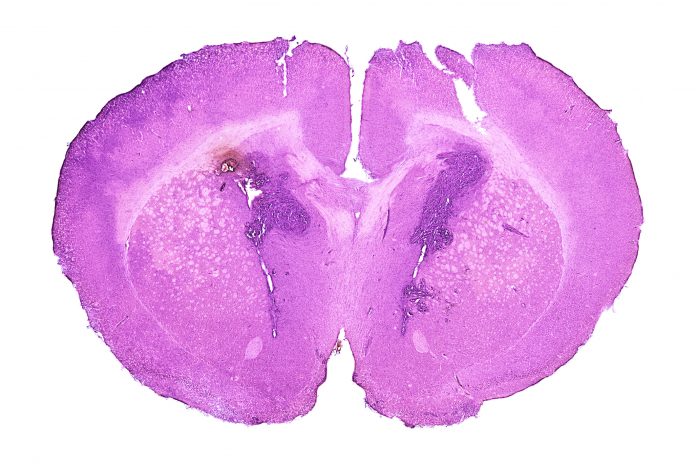
Investigators at Brigham and Women’s Hospital, reporting in the journal Science Translational Medicine, reported that they have developed a microdevice that can help test treatments for glioma, a form of cancer that originates in the spinal chord or brain. The researcher say that the device, which is roughly the same shape and size as a grain of rice, can be used during standard of care surgery to provide new insights on the effect of drugs used to treat gliomas. Use of the device showed no adverse effects in patients during a Phase I clinical trial.
“In order to make the greatest impact on how we treat these tumors, we need to be able to understand, early on, which drug works best for any given patient,” said co-principal investigator and co-corresponding author Pierpaolo Peruzzi, MD, PhD, an assistant professor in the Department of Neurosurgery at Brigham and Women’s Hospital. “The problem is that the tools that are currently available to answer this question are just not good enough. So we came up with the idea of making each patient their own lab, by using a device which can directly interrogate the living tumor and give us the information that we need.”
Use of the device promises to provide unprecedented insight to the effectiveness of treating gliomas, one of the deadliest brain cancers. Developing targeted treatments for gliomas has been challenging since it is difficult to test combination therapies, since patients can only be treated with one approach at a time.
The device, which is implanted in a patient’s tumor tumor during surgery, then removed before the surgery is completed, stays in the tumor for between two to three hours. In that time, it can deliver very small doses of as many as 20 drugs directly into very small areas within the tumor. When the device is removed, the surgeons also remove tissue surrounding the device to be sent to the lab for testing.
“It’s important that we are able to do this in a way that best captures the features of each patient’s tumor and, at the same time, is the least disruptive of the standard of care,” says Peruzzi. “This makes our approach easy to integrate into patients’ treatment and allows its use in real life.”
Since the device works before the tumor has been surgically removed, it provides vital information about how the drugs being tested work within the tumor microenvironment, those cells that directly surround cancer cells and make up nearly 50% of a tumor mass.
Petri notes this provides direct information on how treatments are working. “This is not in the lab, and not in a petri dish, it’s actually in real patients in real time, which gives us a whole new perspective on how these tumors respond to treatment.”
The Phase I study of the device involved a small cohort of six patients. The team reported no adverse events as a result of implanting the device during surgery, and were able to collect data indicating changes in the tumor based on different drug concentrations, along with molecular changes in the cells cause by the drugs. While these first steps in patients showed the device was well tolerated, the investigators will need to figure out exactly what data they want to collect in order to improve glioma treatments. The team is also now testing an approach that takes a minimally invasive approach to implanting the device in the tumor 72 hours before the tumor resection.
“We’re optimistic that this is a new generation approach for personalized medicine,” Peruzzi concludes. “The ability to bring the lab right to the patient unlocks so much potential in terms of the type of information we can gather, which is new and exciting territory for a disease that has very few options at present.”













