In a significant breakthrough, the first MYC inhibitor, OMO-103, has demonstrated both safety and promising anti-tumor activity in a phase I clinical trial led by the Vall d’Hebron Institute of Oncology (VHIO) in Spain.
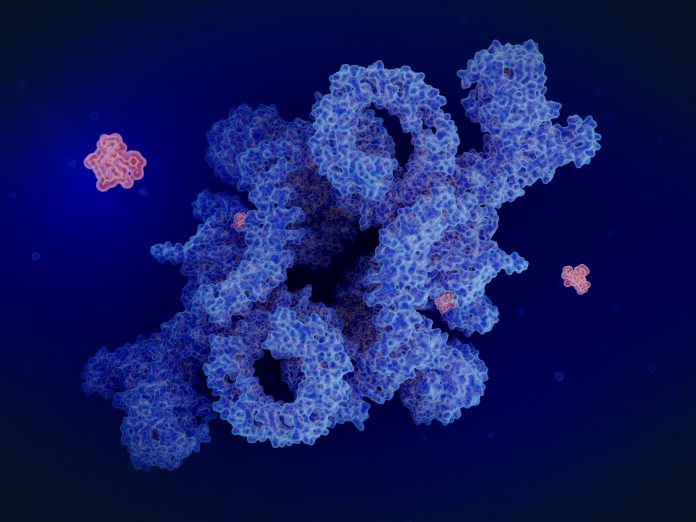
The MYC oncogene has long been recognized as a key player in cancer development, yet until now, it has remained notoriously difficult to target. Developed by the VHIO-born spin-off company Peptomyc, OMO-103 represents a novel approach to inhibiting MYC. Unlike previous attempts, OMO-103 is a mini-protein that has shown the ability to enter cells and reach its target within the nucleus, making it the first clinically viable MYC inhibitor.
Led by Laura Soucek, an ICREA research professor at VHIO, the Phase I trial enrolled 22 patients with advanced metastatic cancer who had exhausted all other treatment options. The results, published in Nature Medicine, were promising, with OMO-103 demonstrating an excellent safety profile and early signs of anti-tumor activity. Notably, some patients experienced disease stabilization and even tumor reduction, offering hope for those facing aggressive and treatment-resistant cancers.
Elena Garralda, director of VHIO’s Research Unit for Molecular Therapy of Cancer, emphasized the importance of these findings. “The main aim of this study was to evaluate the safety of this novel MYC inhibitor,” she explained. “First results demonstrate a favorable safety profile, with only mild side effects including chills and nausea.”
One of the most remarkable observations from the trial was seen in a patient with pancreatic cancer who experienced tumor shrinkage and a reduction in circulating tumor DNA after receiving OMO-103 as fourth-line treatment. Similarly, another patient with a salivary gland tumor remained stable for an impressive 26 months without any adverse events. These results highlight the potential of OMO-103 to offer long-term benefits to patients with otherwise limited treatment options.
Beyond its anti-tumor effects, OMO-103 also shows promise as a tool for identifying biomarkers of response. Soucek and her team identified potential blood-based biomarkers that could help predict which patients are most likely to benefit from treatment with OMO-103. These biomarkers could revolutionize cancer treatment by allowing for more personalized approaches based on individual patient characteristics.
Looking ahead, the researchers are eager to continue investigating the potential of OMO-103 in combination with other therapies. A Phase Ib clinical trial is currently underway to evaluate OMO-103 in combination with standard of care treatments for metastatic pancreatic cancer. These studies represent a crucial step forward in the development of targeted therapies for cancer, offering hope to patients and clinicians alike.
“Our goal is to continue investigating the anti-tumor activity of OMO-103,” Soucek concluded, “to assess its efficacy and potential cooperation with the standard of care in various tumor types.” The researchers believe that with further research and clinical trials, OMO-103 may soon become a vital weapon in the fight against cancer, bringing new hope to patients around the world.













