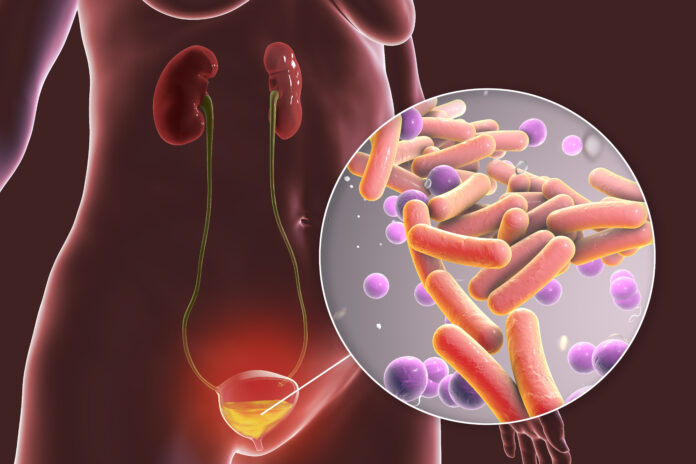
Research in mice shows that previous urinary tract infections (UTIs) can result in bladder remodeling through epigenetic changes that can help fight future infections, but can also result in high levels of inflammation and chronic health issues.
UTIs are an extremely common bacterial infection and can cause significant health problems in women who are otherwise healthy. Recurrence is very frequent, with the strongest risk factor for a UTI being a previous UTI, but the reasons for this are not well understood.
In previous work, lead author of the current Nature Microbiology study Scott Hultgren, a professor at Washington University in St. Louis, and colleagues showed some mice infected with uropathogenic Escherichia coli were able to spontaneously clear their first infection, but others needed antibiotic treatment to do so.
Notably, the mice who spontaneously cleared the first infection could also clear any subsequent infection without help, but the same could not be said for the mice who needed antibiotic treatment. These mice were genetically identical so the researchers reasoned the differences may have another cause.
In the current study, Hultgren and team compared stem cells taken from the lining of the urinary tract (urothelial stem cells) from both groups of mice. They found that epigenetic markers in the mice were triggered by the UTI infections to increase the expression of genes involved in the immune response to infection.
“Epigenetic marks in urothelial stem cells from chronically infected mice enhanced caspase-1-mediated cell death upon uropathogenic E. coli infection, promoting bacterial clearance,” write the authors. Caspase 1 is an enzyme that plays an important role in the inflammatory immune response.
However, while this improved the ability of the mice to fight off the infections, levels of another enzyme, prostaglandin-endoperoxide synthase 2 (Ptgs2os2), also increased. Ptgs2os2 is the mouse version of PTGS2 (COX-2), which is an early protein in a pathway triggering inflammation in humans and the researchers think it may be responsible for the bladder inflammation and mucosal wounding seen in recurrent UTI cases.
“In contrast with adaptive immunity, which encompasses antigen-specific responses by T and B lymphocytes, ‘trained immunity’ is characterized by antigen non-specific tissue adaptation to acute and chronic inflammation, sometimes in response to infection,” write the authors.
“Our discovery of epithelial stem cell epigenetic reprogramming upon uropathogenic E. coli infection has implications for understanding the mechanism of epithelial-intrinsic trained immunity against not only UTIs, but also other types of infection or inflammatory disease,” they add, although they caution than more research to confirm their findings in humans is needed.













