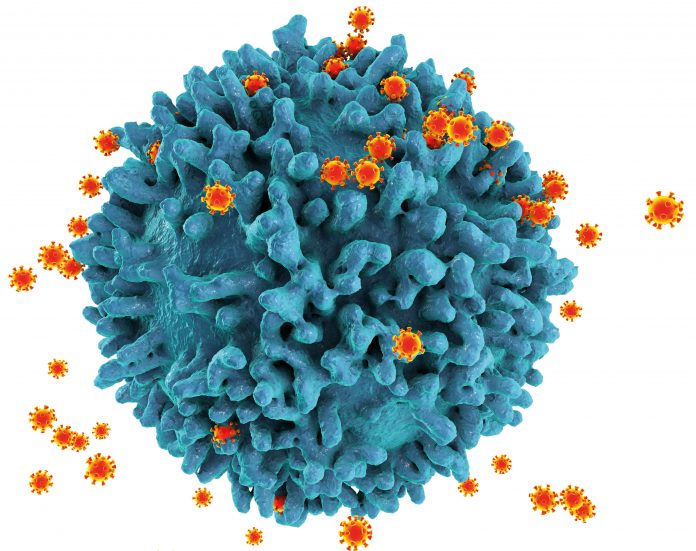
Researchers from Fred Hutchinson Cancer Center, Scripps Research, and The International AIDS Vaccine Initiative (IAVI) report that the Phase I IAVA G001 clinical trial to test the safety and immune response of a self-assembling nanoparticle HIV vaccine has exhibited a strong T-cell response in human subjects. The data from the trial, published in the journal Science Translational Medicine, represents a major step forward in the effort to develop a vaccine to address the worldwide HIV/AIDS epidemic.
“We were quite impressed that this vaccine candidate produced such a vigorous T-cell response in almost all trial participants who received the vaccine,” said the study’s co-senior author Julie McElrath, MD, PhD, senior vice president and director of Fred Hutch’s Vaccine and Infectious Disease Division. “These results highlight the potential of this HIV-1 nanoparticle vaccine approach to induce the critical T-cell help needed for maturing antibodies toward the pathway of broadly neutralizing against HIV.”
The antigen used in the study, which was jointly developed by IAVI and Scripps, was previously shown to stimulate VRC01-class B cells, an immune response considered promising for informing additional studies. The new clinical study, McElrath noted, is only the first step as a heterologous booster vaccine will still be needed to produce VRC01-class broadly neutralizing antibodies shown to neutralize roughly 90% of existing HIV strains in previous studies.
The newest study was a Phase I, randomized, double-blind and placebo controlled clinical trial designed to test the safety and effectiveness of the nanoparticle vaccine in health volunteers. The 48 total enrollees were broken up into two groups with 18 receiving the vaccine and six receiving placebo in each group. Vaccine recipients received two doses of the vaccine with eight weeks between doses.
Key findings include:
- Vaccine-specific CD4 T cells were induced in almost all vaccine recipients;
- Lymph node GC T follicular helper cells increased after vaccination compared to placebo;
- Lumazine synthase protein, needed for self-assembly of the particle, also induced T-cell responses that can provide additional help to ultimately enhance efficacy in a sequential vaccine strategy:
- Vaccine-specific CD4 T cells were polyfunctional and had diverse phenotypes;
- LumSyn-specific CD8 T cells were highly polyfunctional and had a predominantly effector memory phenotype;
- CD4 T-cell responses were driven by immunodominant epitopes with diverse and promiscuous HLA restriction; and
- CD8 T-cell responses to LumSyn were driven by HLA-A*02-restricted immunodominant epitopes B- and T-cell responses correlated within but not between LN and peripheral blood compartments.
“We showed previously that this vaccine induced the desired B-cell responses from HIV broadly neutralizing antibody precursors. Here we demonstrated strong CD4 T-cell responses, and we went beyond what is normally done by drilling down to identify the T cell epitopes and found several broadly immunogenic epitopes that might be useful for developing boosters and for other vaccines,” said William Schief, PhD, executive director of vaccine design for IAVI’s Neutralizing Antibody Center at Scripps Research and co-senior author of the study.













